Litigation Guides
Traumatic Brain Injuries Resulting From Motor Vehicle Accidents
Motor vehicle accidents can cause a range of brain injuries, from obvious to insidious, including tears in the long cables of nerve cells connecting different regions of the brain, intracranial bleeding, and long-term psychiatric changes. While the causes of moderate to severe traumatic brain injuries (TBIs) are well-understood, mild TBIs (mTBIs), also known as concussions, are less well-understood.1
Written By
Wendy Ketner, M.D.
Medically Reviewed
What is a Traumatic Brain Injury?
Definition
The annual incidence of mTBIs is estimated to be 600 per 100,000 people. A Traumatic Brain Injury (TBI) is defined as an alteration in brain function or other evidence of brain damage caused by an external force, such as:2
- The head striking or being struck by an object
- The brain undergoing an acceleration/deceleration movement without direct external trauma to the head (e.g., whiplash)
- A foreign body penetrating the brain
- Forces generated from vents such as a blast or explosion
- Other forces yet to be identified
Alterations in Brain Function
Alterations in brain function include:2
- Any period of loss or decreased level of consciousness (LOC)
- Any loss of memory for events immediately before (retrograde amnesia) or after the injury (post-traumatic amnesia)
- Focal neurological deficits (loss of balance, change in vision, dyspraxia [where a person has difficulty planning and coordinating the movements needed to perform purposeful actions], paresis/ plegia [weakness or paralysis of one or more limbs], sensory loss, aphasia [difficulting comprehending or producing speech], etc.)
- Alteration in mental state at the time of the injury (i.e., confusion, disorientation, slowed thinking, etc.).
How are Traumatic Brain Injuries Diagnosed?
Soft Tissue Brain Damage
Different testing modalities, including the Glasgow Coma Scale (GCS) score, imaging, and clinical biomarkers, have been used to help diagnose moderate and severe TBIs. Computed tomography (CT) or magnetic resonance imaging (MRI) are the mainstays for assessing soft tissue damage to the brain such as:3
- Cerebral Contusion: A bruise on the brain's surface.
- Subdural Hematoma: A collection of blood between the brain and its outermost covering.
- Epidural Hematoma: Accumulation of blood between the skull and the brain's protective lining
- Traumatic Subarachnoid Hemorrhage: Bleeding into the space between the brain and its protective membranes.
- Shearing Injury and Diffuse Axonal Injury: Brain injuries caused by severe head movement or shaking, leading to damage of nerve fibers throughout the brain.
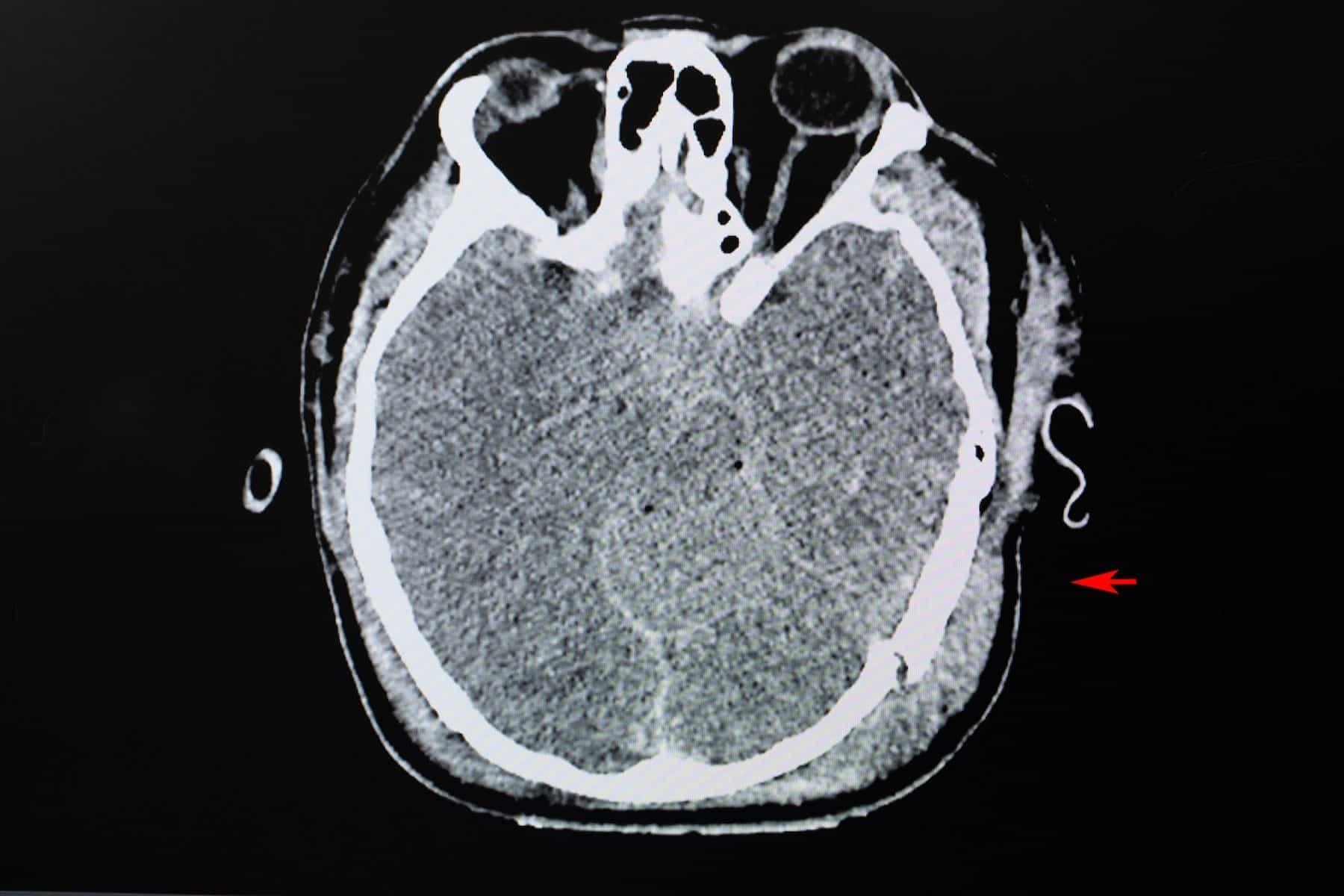
Skull Fractures
Skull fractures resulting from TBIs are generally assessed using CT scans of the head and include:3
- Linear Skull Fracture: A break in the skull bone that follows a straight line, often without bone displacement.
- Depressed Skull Fracture: A skull bone break where a part of the bone is pushed inward, toward the brain.
- Basilar Skull Fracture: A fracture at the base of the skull, typically involving the bones near the brain's bottom.
- Penetrating Skull Fracture: A fracture that results from an object piercing through the skull, potentially damaging the brain.
Speak with a neurology expert about your case
What are the long-term outcomes of TBIs and mTBIs?
Major Issues
Because the brain has such a vast spectrum of responsibilities, the long-term sequelae of TBI can be broad-reaching. Some major issues facing those who have suffered from TBI are:4
- Mental health - including depression, anxiety, schizophrenia
- Intellectual - including cognitive impairment and personality and behavior changes
- Lifestyle - including quality of life, functional status, and substance use disorder
- Physical - including seizures and somatic complaints, such as headaches
Diagnostic Features
While a general classification of TBI severity is usually correlated with prognosis, it is better to assess the potential long-term neurological outcome by examining each sign and symptom individually. Specific diagnostic features have a greater impact on future neurological consequences. These features can include:5
- Intraventricular hemorrhage: Bleeding inside the brain's fluid-filled chambers, called ventricles.
- Ischemic Brain Injury: Damage to the brain due to reduced blood flow, often caused by a clot or blockage.
- Diffuse Axonal Injury: Widespread brain injury affecting nerve fibers, usually from rapid head movement.
- Elevated ICP (Intracranial Pressure): Increased pressure inside the skull, which can be a sign of brain swelling or other issues.
- Midline Shift: Displacement of brain structures from their normal position, indicating pressure or swelling.
- Sulcal Effacement: Flattening or narrowing of the spaces between brain folds (sulci), often due to swelling.
- Contusions: Brain bruises or damaged areas resulting from impact or injury
Mild TBIs
Over 90% of TBI cases are classified as mild. Mild TBI (mTBI) is frequently viewed as transient and benign, with expectations of quick symptom resolution within days. However, this oversimplifies the complexity of mTBI, and the following points are important to remember:6
- It spans a broad range of injury severity and underlying pathological processes.
- Up to 30% report ongoing symptoms at 3 months post-injury.
- Persistent symptoms significantly affect occupational and social functioning.
- Various non-brain injury factors may also contribute to chronic complaints.
- Repeated mild TBIs increasingly link to later neurodegenerative disease.
Strength of Available Evidence
Association between TBI, including mild TBI, and long-term mental health, cognitive, and physical symptoms.
- HIGH
- Evidence supporting this topic is robust
Works Cited
1.
Morin M, Langevin P, Fait P. Cervical Spine Involvement in Mild Traumatic Brain Injury: A Review. Journal of Sports Medicine. Published online 2016:1-20. URL
2.
Menon DK, Schwab K, Wright DW, Maas AI. Position Statement: Definition of Traumatic Brain Injury. Archives of Physical Medicine and Rehabilitation. 2010;91(11):1637-1640. URL
3.
Pervez M, Kitagawa RS, Chang TR. Definition of Traumatic Brain Injury, Neurosurgery, Trauma Orthopedics, Neuroimaging, Psychology, and Psychiatry in Mild Traumatic Brain Injury. Neuroimaging Clinics of North America. 2018;28(1):1-13. URL
4.
Trevena L, Cameron I. Traumatic brain injury - long term care of patients in general practice. Australian Family Physician. 2011;40(12):956-961. Accessed October 3, 2023. URL
5.
Baxendale S, Heaney D, Rugg-Gunn F, Friedland D. Neuropsychological outcomes following traumatic brain injury. Practical Neurology. 2019;19(6):476-482. URL
6.
Jenkins PO. Persistent symptoms after a mild traumatic brain injury: assessment and management. Medicine. 2023;51(8):581-585. URL
About the author
Wendy Ketner, M.D.
Dr. Wendy Ketner is a distinguished medical professional with a comprehensive background in surgery and medical research. Currently serving as the Senior Vice President of Medical Affairs at the Expert Institute, she plays a pivotal role in overseeing the organization's most important client relationships. Dr. Ketner's extensive surgical training was completed at Mount Sinai Beth Israel, where she gained hands-on experience in various general surgery procedures, including hernia repairs, cholecystectomies, appendectomies, mastectomies for breast cancer, breast reconstruction, surgical oncology, vascular surgery, and colorectal surgery. She also provided care in the surgical intensive care unit.
Her research interests have focused on post-mastectomy reconstruction and the surgical treatment of gastric cancer, including co-authoring a textbook chapter on the subject. Additionally, she has contributed to research on the percutaneous delivery of stem cells following myocardial infarction.
Dr. Ketner's educational background includes a Bachelor's degree from Yale University in Latin American Studies and a Doctor of Medicine (M.D.) from SUNY Downstate College of Medicine. Moreover, she is a member of the Board of Advisors for Opollo Technologies, a fintech healthcare AI company, contributing her medical expertise to enhance healthcare technology solutions. Her role at Expert Institute involves leveraging her medical knowledge to provide insights into legal cases, underscoring her unique blend of medical and legal acumen.
Subscribe to our newsletter
Join our newsletter to stay up to date on legal news, insights and product updates from Expert Institute.
Speak with a Neurology Expert
We're here to help you build a stronger case. Retain a leading expert witness today.
- Access tailored expertise on every case
- Trust your expert immediately
- Speak with your expert before retaining
Need your medical records reviewed? Consult one of our 75+ on-staff physicians who can help evaluate the strengths and weaknesses of your case.
Need your medical records reviewed? Consult one of our 75+ on-staff physicians who can help evaluate the strengths and weaknesses of your case.


