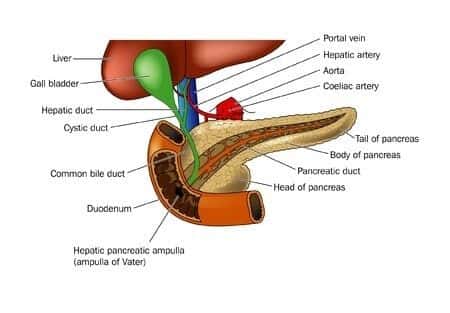
This case takes place in Missouri and involves a 59 year old male who presented to his PCP with signs of obstructive jaundice. His primary care physician refers him for a CT scan and the initial CT scan showed a mass in the uncinate process of the pancreas measuring 3.0 x 3.4 x 1.9 highly suspicious for neoplasm with some mild intrahepatic biliary dilation. PCP indicated that patient likely has a carcinoma in the head of the pancreas in the uncinate process causing obstruction. He was told he needed further evaluation and may need a needle-guided biopsy. The patient was admitted 5 days later and a whipple procedure was performed. Pathology results revealed that no masses or nodules are identified. No grossly identified tumor. The pancreatic neck, common bile duct, unicate margin and proximal duodenal margin were all negative for malignant cells. After more prudent workup post operatively the patient was found to have autoimmune pancreatitis.
Question(s) For Expert Witness
Did the pancreatic surgeon breach the applicable standard of care by not conducting a proper work up of the case to rule out autoimmune pancreatitis before he rendered a diagnoses of “distal cholangiocarcinoma” and performed the whipple procedure on the patient? Would these tests have been performed in normal circumstances to rule out an autoimmune etiology before resorting to life altering surgery?
Expert Witness Response E-000233
There are several studies that should be done before jumping to conclusions and performing a very difficult surgery that carries a very high mortality rate. Endoscopic ultrasonography (EUS) and/or fine-needle aspiration (FNA) are occasionally performed in a patient who is being considered for pylorus-preserving pancreaticoduodenectomy (PPPD) (Whipple procedure). Although not routinely employed, EUS is helpful when pancreatic head masses are poorly detected on CT imaging. Tumor aspiration is not routinely employed for preoperative tissue diagnosis, because FNA results do not affect surgical decision making; however, confirmation of malignancy can be useful in the setting of neoadjuvant therapy. Also, there is a finite risk of seeding the peritoneum with malignant disease from needle biopsy. If there was no ERCP done prior to surgery and no needle biopsy to search for an underlying pathology then I can't really agree with the steps taken by the surgeon on this case.
About the author
Michael Talve, CEO
Michael Talve stands at the forefront of legal innovation as the CEO and Managing Director of Expert Institute. Under his leadership, the Expert Institute has established itself as a vital player in the legal technology arena, revolutionizing how lawyers connect with world-class experts and access advanced legal technology. Michael's role involves not only steering the company's strategic direction but also ensuring the delivery of unparalleled intelligence and cutting-edge solutions to legal professionals. His work at Expert Institute has been instrumental in enhancing the capabilities of attorneys in case preparation and execution, making a significant impact on the legal industry's approach to expert consultation and technological integration. Michael's vision and execution have positioned the Expert Institute as a key facilitator in the intersection of law and technology.