This case involves a fourteen-year-old male who presented to the emergency room with symptoms of a seizure. His parents said that he was walking in their house when he began to smell burning rubber. A few seconds later, he dropped to the ground and started to convulse. Testing was performed, which showed that the boy had a focal seizure confined to the frontal lobe of the brain. After he was given IV lamotrigine, his symptoms began to dissipate. However, over the next few hours, the patient started to develop a fever, sore throat, and fatigue. The emergency room physician believed that he developed a hospital-acquired infection and initiated him on antibiotics. One hour later, the boy’s symptoms became worse, accompanied by ulcer formation on his lips and inside his mouth. The patient’s condition rapidly declined, evidenced by low blood pressure and elevated heart rate. His family was told that he developed a serious skin condition known as Stevens-Johnson syndrome secondary to lamotrigine. The boy received IV fluids and pain management which helped but didn’t alleviate the ulcers. He began to develop ulcers throughout his whole body requiring emergent surgical debridement. The boy survived but had lifelong physical disfigurement from the ulcers.
Question(s) For Expert Witness
1. Did this emergency room physician follow the standard of care when prescribing lamotrigine, and what should have been done to prevent further harm in this patient?
Expert Witness Response
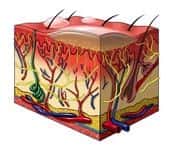
Lamotrigine is a medication that is commonly used to treat focal seizures. A focal seizure is classified as a seizure that is localized to one lobe of the brain. This physician properly treated the boy’s seizure. However, when he began to develop signs of Stevens-Johnson syndrome the emergency room doctor falsely believed that he developed an infection. Although this was possible, it would be uncommon for such an infection to develop at a rapid rate. Stevens-Johnson syndrome is a potentially fatal skin condition that does develop rapidly. Patients will quickly develop fever, sore throat, and fatigue. Shortly after, ulcerations begin to form in the mucous membranes which include the eyes, mouth, lips, nose, genitals, and anus. Giving this boy antibiotics under the impression of an infection may have actually exacerbated the Stevens-Johnson syndrome; especially if the antibiotic contained sulfur. Proper treatment of Stevens-Johnson syndrome includes intravenous fluids and pain management. If the ulcer formation is severe, surgical debridement may be required. An even more severe form of Stevens-Johnson syndrome is known as toxic epidermal necrolysis. The mortality rates for these two conditions are as high as 5% and 40%, respectively.
About the author
Jason Cohn
Jason is a 4th year medical student pursuing a career in Otolaryngology/Facial Plastic Surgery. His Interest include sports, fitness, chemistry, otolaryngology, plastic surgery, allergy/immunology, surgical oncology, human genetics, public health, preventative medicine, and rheumatology.