Neurosurgery Expert Advises On Post-Operative Paralysis
Updated on
Case Overview
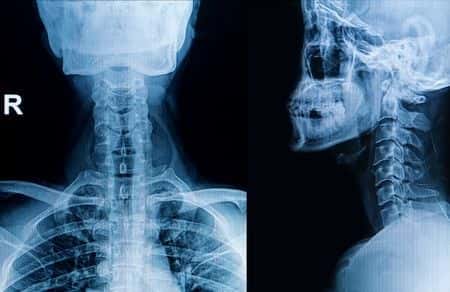
This case involves a male patient, located in West Virginia, who had a past medical history of Cervical myelopathy and multilevel cervical radiculopathy which was suspected to be caused by cervical cord compression. He was recommended for surgery and was taken off his anticoagulants in preparation. The patient underwent a decompressing cervical laminectomy. A hemovac drain was placed in the epidural space. The next day the patient had regained some strength and was sitting up. His anticoagulants (Lovenox were restarted. The patient’s hemovac drain was removed. Three-days later the patient was walking and suffered a sudden loss of sensation in all extremities. The patient had acute respiratory failure and a Code Blue was initiated. He was intubated and transferred to ICU at which point the records state that he was quadriplegic. An MRI of the cervical spine was performed that evening which revealed: “Interval laminectomies from C3-C7 since prior MRI with posterior paraspinous hematoma at midline extending along these levels. STAT CALL, CRITICAL FINDING.” Two-hours later the patient was taken to the OR to evacuate the spinal epidural hematoma. Ten-hours had elapsed since the patient had first showed signs of a neurological complication. Post-operatively, the patient had no movements from the neck down and required mechanical ventilation.
Questions to the Neurosurgery expert and their responses
How often do you treat patients with this presentation?
This case fits my specific area of expertise very well. I treat patients with this presentation very often. My practice is primarily involved with cervical spine surgery, and I have a great deal of experience with cervical myelopathy and radiculopathy.
Could the timing of the intervention over 10 hours from onset have contributed to the paralysis?
The timing of the intervention could possibly have contributed to the paralysis, depending on what was happening with the patient's condition in those 10 hours.
About the expert
This board certified neurosurgeon specializes in cervical spine surgery. He earned a BA in Neurobiology from the University of California Berkeley and an MD from UCLA School of Medicine. He completed internship training in general surgery at Washington University, residency training in neurosurgery at Washington University where he served as chief resident, and fellowship training in spinal neurosurgery at Cedars Sinai Medical Center and UCLA School of Medicine. He is a member of numerous prestigious societies in the neurosurgery field, and has authored more than 30 publications in regards to spinal neurosurgery. He is a former assistant professor of neurological surgery at Washington University. Currently, this expert serves as a distinguished professor of neurological surgery and an associate professor of neurological/orthopaedic surgery at one of the nation's top university medical centers. He also practices at two area hospitals in the field of spinal neurosurgery.

E-009297
Specialties:
Subscribe to our newsletter
Join our newsletter to stay up to date on legal news, insights and product updates from Expert Institute.
Sign up nowFind an expert witness near you
What State is your case in?
Subscribe to our newsletter
Join our newsletter to stay up to date on legal news, insights and product updates from Expert Institute.