Neurologist’s Workup of Stroke Patient Contributes to Cerebral Death
Updated on
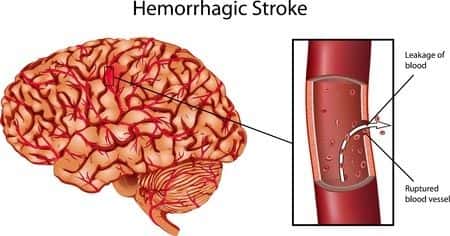
This case involves a seventy-seven-year-old woman with a medical history of hypertension, hyperlipidemia, and infrequent palpitations who presented to the hospital with an acute onset of slurred speech. The patient arrived outside of the window period for the administration of tPA and doctors advised that no other medical intervention was indicated other than supportive care. Subsequently, the patient was admitted to the stroke unit for further observation but at no time was an EKG, neuroradiology, or any other cardiac testing performed to rule out an embolism as the cause of the stroke. Three days into her hospital stay, the patient again displayed significant signs of stroke and was no longer able to support her own airway. She was placed on a ventilator and further brain imaging showed extensive cerebral damage consistent with brain death. The patient’s family elected to remove her from the respirator and she died shortly thereafter.
Question(s) For Expert Witness
1. What additional tests could have been performed to alter this patient's outcome?
Expert Witness Response E-000197
 This patient had a history of palpitations. Although infrequent, her palpitations should have raised the suspicion of a possible arrhythmia as a cause of her stroke. Because paroxysmal atrial fibrillation (PAF) episodes are often subclinical, ambulatory ECG monitoring was a reasonable additional evaluation in this patient and may have helped to prevent the fatal embolism.
This patient had a history of palpitations. Although infrequent, her palpitations should have raised the suspicion of a possible arrhythmia as a cause of her stroke. Because paroxysmal atrial fibrillation (PAF) episodes are often subclinical, ambulatory ECG monitoring was a reasonable additional evaluation in this patient and may have helped to prevent the fatal embolism.
About the author
Michael Talve, CEO
Michael Talve stands at the forefront of legal innovation as the CEO and Managing Director of Expert Institute. Under his leadership, the Expert Institute has established itself as a vital player in the legal technology arena, revolutionizing how lawyers connect with world-class experts and access advanced legal technology. Michael's role involves not only steering the company's strategic direction but also ensuring the delivery of unparalleled intelligence and cutting-edge solutions to legal professionals. His work at Expert Institute has been instrumental in enhancing the capabilities of attorneys in case preparation and execution, making a significant impact on the legal industry's approach to expert consultation and technological integration. Michael's vision and execution have positioned the Expert Institute as a key facilitator in the intersection of law and technology.
Subscribe to our newsletter
Join our newsletter to stay up to date on legal news, insights and product updates from Expert Institute.
Sign up nowFind an expert witness near you
What State is your case in?
Subscribe to our newsletter
Join our newsletter to stay up to date on legal news, insights and product updates from Expert Institute.