Man Suffers Brain Damage Due to Oxygen Starvation While on Ventilator
Updated on
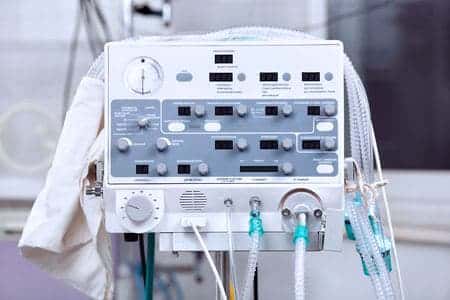
This case involves a man who was admitted to a hospital in Nebraska for treatment of severe pneumonia and was put on a ventilator. Initially, he responded well to treatment, and was plans were made for him to be discharged. However, hours before he was due to be discharged, he developed a sudden drop in his oxygen saturation. A nurse responded and suctioned the patient, and a respiratory therapist was called to assess and manage the airway. While managing the airway it is alleged that the respiratory therapist failed to monitor the patient’s vital signs, and his heart rate dropped and he went into respiratory arrest. Despite being successfully resuscitated he sustained brain damage from oxygen starvation.
Question(s) For Expert Witness
1. How often do you treat patients like the one described?
2. What type of monitoring is required when assessing and managing a patient's airway?
Expert Witness Response E-007056
 I have been an educator since 1994, and have taught respiratory care for 11 years, and managed my hospital's respiratory care area as an Associate Director of the Respiratory Care Department at a major university hospital for 8 years. Patients on mechanical ventilation should be on electronic monitoring of oxygen saturation, respiratory and heart rate, and temperature and blood pressure. Respiratory therapists must also be involved in routine ventilator checks, which would include: review of all monitored patient parameters (vital signs, oxygen saturation); patient assessment (listening to lung and heart sounds, chest movement, secretions, color); a complete check of all ventilator settings, alarms, and ventilator monitored parameters; plus any humidification or medication therapy. Many of the cases involved patient monitoring issues stemming from setup and monitoring of a transport ventilator, weaning from mechanical ventilation, failure to notice signs of respiratory failure.
I have been an educator since 1994, and have taught respiratory care for 11 years, and managed my hospital's respiratory care area as an Associate Director of the Respiratory Care Department at a major university hospital for 8 years. Patients on mechanical ventilation should be on electronic monitoring of oxygen saturation, respiratory and heart rate, and temperature and blood pressure. Respiratory therapists must also be involved in routine ventilator checks, which would include: review of all monitored patient parameters (vital signs, oxygen saturation); patient assessment (listening to lung and heart sounds, chest movement, secretions, color); a complete check of all ventilator settings, alarms, and ventilator monitored parameters; plus any humidification or medication therapy. Many of the cases involved patient monitoring issues stemming from setup and monitoring of a transport ventilator, weaning from mechanical ventilation, failure to notice signs of respiratory failure.
About the author
Wendy Ketner, M.D.
Dr. Wendy Ketner is a distinguished medical professional with a comprehensive background in surgery and medical research. Currently serving as the Senior Vice President of Medical Affairs at the Expert Institute, she plays a pivotal role in overseeing the organization's most important client relationships. Dr. Ketner's extensive surgical training was completed at Mount Sinai Beth Israel, where she gained hands-on experience in various general surgery procedures, including hernia repairs, cholecystectomies, appendectomies, mastectomies for breast cancer, breast reconstruction, surgical oncology, vascular surgery, and colorectal surgery. She also provided care in the surgical intensive care unit.
Her research interests have focused on post-mastectomy reconstruction and the surgical treatment of gastric cancer, including co-authoring a textbook chapter on the subject. Additionally, she has contributed to research on the percutaneous delivery of stem cells following myocardial infarction.
Dr. Ketner's educational background includes a Bachelor's degree from Yale University in Latin American Studies and a Doctor of Medicine (M.D.) from SUNY Downstate College of Medicine. Moreover, she is a member of the Board of Advisors for Opollo Technologies, a fintech healthcare AI company, contributing her medical expertise to enhance healthcare technology solutions. Her role at Expert Institute involves leveraging her medical knowledge to provide insights into legal cases, underscoring her unique blend of medical and legal acumen.
Subscribe to our newsletter
Join our newsletter to stay up to date on legal news, insights and product updates from Expert Institute.
Sign up nowFind an expert witness near you
What State is your case in?
Subscribe to our newsletter
Join our newsletter to stay up to date on legal news, insights and product updates from Expert Institute.